Tilt: Causes and Solutions
Lower back pain affects millions of people worldwide, becoming one of the most common reasons individuals seek medical attention. Among the various causes, an improper pelvic tilt stands out as a significant yet frequently overlooked contributor. The relationship between lower back pain and pelvic alignment is complex but understanding this connection can provide invaluable insights for those suffering from chronic discomfort. When the pelvis shifts from its neutral position, it places excessive strain on the lumbar spine, potentially leading to persistent pain, reduced functionality, and a diminished quality of life.
Many people attempt to address their lower back pain through generic solutions without realizing that the root cause might be directly related to their pelvic positioning. This oversight often results in temporary relief rather than lasting improvement. By exploring the intricate relationship between pelvic alignment and spinal health, individuals can take more targeted approaches to alleviate their discomfort and prevent future occurrences.
The Connection Between Lumbar Lordosis and Pelvic Alignment
The lumbar spine naturally features a slight inward curve, known medically as lumbar lordosis. This natural curvature plays a crucial role in absorbing shock, maintaining balance, and facilitating smooth movement patterns throughout daily activities. However, when this curve becomes exaggerated due to a tilted pelvis, it creates a cascade of compensatory adjustments throughout the entire kinetic chain.
An anterior pelvic tilt typically increases lumbar lordosis, while a posterior tilt flattens it. Both scenarios shift the spine away from its optimal alignment, placing uneven pressure on vertebral discs, facet joints, and surrounding soft tissues. Over time, these pressures can manifest as degenerative changes in the lumbar spine, contributing to conditions ranging from muscle strains to herniated discs.
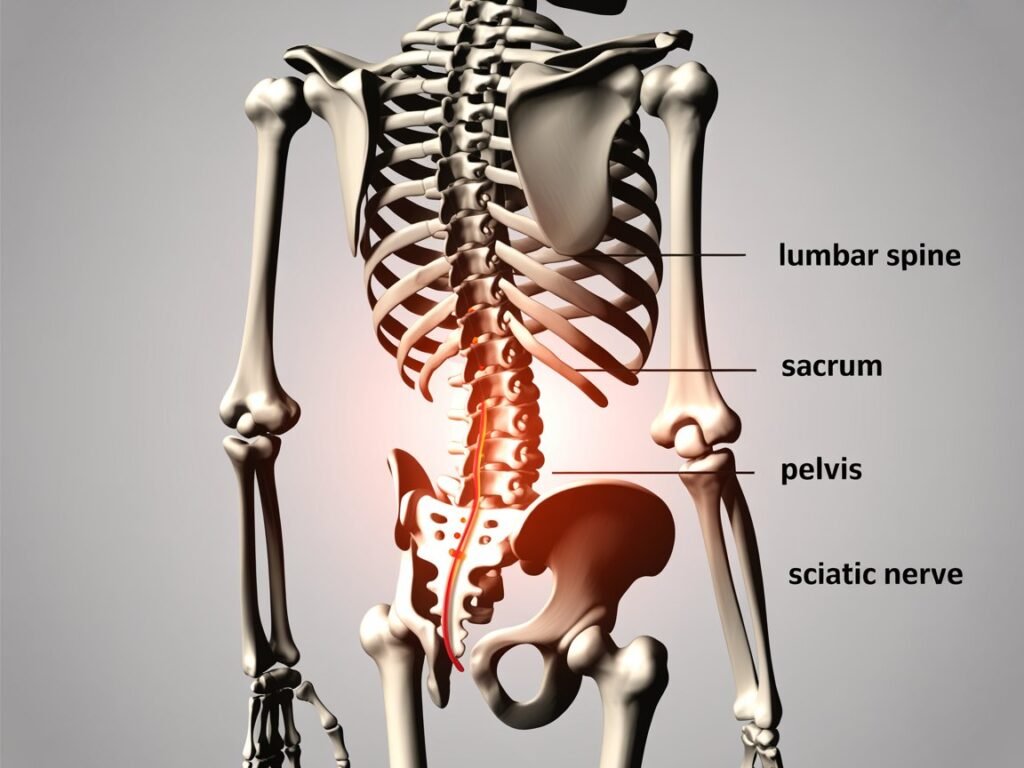
The relationship works both ways—issues originating in the lumbar spine can also affect pelvic positioning. This interdependence highlights the importance of addressing both regions simultaneously rather than focusing exclusively on one area. A skilled physical therapist can accurately assess this relationship by examining how movement patterns in one area influence the other, providing valuable insights for treatment planning.
Common Causes of Abnormal Pelvic Tilt
Several factors contribute to developing an abnormal pelvic position, many of which relate to modern lifestyle habits:
Muscular Imbalances
One primary cause involves tight hip flexors, particularly the psoas and iliacus muscles. These muscles connect the lumbar spine to the femur and, when chronically shortened from prolonged sitting, pull the pelvis into an anterior tilt. This tightness creates a chain reaction that affects the entire postural system.
Simultaneously, weak gluteal muscles fail to provide adequate posterior support for the pelvis. The gluteal complex plays a crucial role in maintaining proper pelvic alignment during both static positions and dynamic movements. When these muscles become deconditioned, they cannot effectively counterbalance the pull from tight anterior muscles.
Lifestyle Factors
Contemporary lifestyles frequently contribute to pelvic misalignment through:
Extended periods of sitting at desks or during commutes
Poor posture habits developed from electronic device usage
Inappropriate footwear choices that alter weight distribution
Repetitive movement patterns from work or recreational activities
Imbalanced exercise routines that strengthen some muscle groups while neglecting others
The upper body position also significantly influences pelvic alignment. Forward head posture and rounded shoulders shift the center of gravity, requiring compensatory adjustments in the pelvis to maintain balance. This interconnection demonstrates how issues seemingly distant from the pelvis can directly impact its positioning.
Structural and Medical Considerations
Beyond lifestyle and muscular factors, certain structural and medical conditions can contribute to pelvic misalignment:
Leg length discrepancies
Previous injuries or surgeries affecting gait patterns
Joint hypermobility or restricted range of motion
Pregnancy and postpartum physical changes
Congenital factors affecting skeletal structure
Understanding these various contributors helps create a more comprehensive treatment plan that addresses root causes rather than just symptoms.
Effective Tilt Exercises for Restoration
Corrective tilt exercises form the cornerstone of rehabilitation for pelvic misalignment. These exercises should progress systematically through awareness, control, and integration phases:
Awareness Phase
The journey begins with developing proprioceptive awareness of the pelvis in space:
Pelvic Clock Exercises: While lying supine, visualize the pelvis as a clock face and practice tilting in different directions to understand current range of motion and identify restricted movements.
Mirror Feedback: Using visual feedback from a side-view mirror to recognize what neutral position actually feels like, as many individuals with chronic misalignment have normalized incorrect positioning.
Wall Standing: Backing against a wall to feel contact points and work on maintaining neutral spine alignment while performing subtle pelvic movements.
These awareness exercises help individuals recognize when their pelvis deviates from neutral position during daily activities, creating the foundation for lasting change.
Strengthening and Mobilization
Once awareness improves, targeted strengthening exercises address specific muscular imbalances:
Posterior Chain Activation: Exercises like bridges, bird-dogs, and deadbug variations strengthen the gluteal muscles and other posterior chain components without compromising lumbar position.
Core Stabilization: Progressive core routines that maintain neutral pelvic alignment while challenging stability from different positions and with various loads.
Hip Flexor Release: Techniques to release tight hip flexors combined with active lengthening exercises to restore optimal tissue length and function.
Integrated Movement Patterns: Compound movements that coordinate upper body and lower body segments while maintaining proper pelvic alignment.
Each exercise should emphasize quality over quantity, focusing on precise execution with proper breathing patterns rather than repetition counts or intensity levels.
Functional Integration
The final phase incorporates improved pelvic control into everyday activities:
Sitting Posture Training: Practicing neutral pelvic alignment during seated activities, potentially using ergonomic supports initially while developing internal control.
Standing Alignment: Techniques for maintaining proper alignment during prolonged standing without reverting to habitual postures that strain the lumbar spine.
Movement Pattern Retraining: Applying correct pelvic positioning during walking, stair climbing, bending, lifting, and other routine activities.
This functional integration phase bridges the gap between isolated exercises and real-world application, making the improvements sustainable long-term.
Seeking Professional Guidance
While self-help exercises can provide benefits, consulting with a qualified physical therapist often proves crucial for optimal outcomes. A professional brings several advantages to the rehabilitation process:
Accurate Assessment
A physical therapist conducts comprehensive evaluations that may include:
Movement screening to identify dysfunctional patterns
Specific muscle length and strength testing
Postural analysis from multiple planes
Functional task assessment
Potential referral for imaging when appropriate
This thorough assessment ensures that treatment addresses the true underlying causes rather than just obvious symptoms.
Customized Treatment Approaches
Based on assessment findings, a physical therapist develops an individualized treatment plan that may incorporate:
Manual therapy techniques to address joint restrictions or tissue adhesions
Specific exercise progressions matched to current capabilities
Neuromuscular re-education strategies
Modalities to manage pain during the rehabilitation process
Education about activity modifications
This personalized approach acknowledges that no two cases of pelvic misalignment are identical, even when symptoms appear similar.
Progression Monitoring
Professional guidance ensures appropriate advancement through rehabilitation stages:
Objective reassessment to document improvements
Timely modification of exercises as capabilities change
Problem-solving when progress plateaus
Maintenance strategies once optimal function returns
This systematic progression maximizes efficiency and effectiveness while minimizing the risk of setbacks from inappropriate exercise selection or advancement.
The Role of Complementary Approaches
While exercise-based interventions form the foundation of pelvic alignment correction, several complementary approaches can enhance outcomes:

Ergonomic Modifications
Environmental adjustments support postural improvements:
Workstation setup optimization
Appropriate mattress and pillow selection
Car seat adjustments for driving comfort
Tool modifications for occupational tasks
These modifications reduce environmental barriers to maintaining proper alignment throughout daily activities.
Mind-Body Techniques
Several practices enhance body awareness and movement quality:
Tai Chi and Qigong for dynamic control
Pilates for precision movement
Yoga for mobility and stability (with appropriate modifications)
Feldenkrais or Alexander Technique for movement efficiency
These approaches complement traditional exercises by enhancing proprioception and movement consciousness.
Maintaining Long-Term Spinal Health
After addressing acute symptoms and establishing better alignment patterns, maintaining these improvements becomes the priority. This maintenance phase involves several key components:
Ongoing Self-Assessment
Regular self-checks help identify subtle regressions before they become problematic:
Periodic posture photos or videos for visual feedback
Mindfulness of sensation during routine activities
Recognition of early warning signs that previously preceded pain episodes
Monitoring changes in range of motion or comfort levels
This self-awareness creates opportunities for early intervention rather than waiting until problems become severe.
Sustainable Exercise Routines
Long-term spinal health depends on balanced physical activity that:
Maintains adequate strength in all muscle groups surrounding the pelvis
Preserves appropriate range of motion through regular mobility work
Incorporates variety to prevent overuse patterns
Focuses on movement quality rather than just quantity or intensity
These ongoing movement practices prevent the recurrence of imbalances that initially contributed to the tilted pelvis and subsequent lower back pain.
Lifestyle Integration
Ultimately, spinal health depends on integrating proper mechanics into everyday life:
Maintaining awareness of pelvic position during prolonged postures
Applying proper body mechanics for lifting and carrying tasks
Taking regular movement breaks during sedentary periods
Balancing activity types to avoid repetitive stresses
This holistic approach acknowledges that spinal health extends beyond formal exercise sessions into every aspect of daily living.
Conclusion
The relationship between lower back pain and pelvic tilt represents a critical but often overlooked connection in musculoskeletal health. By understanding how a tilted pelvis affects the lumbar spine and overall function, individuals can take more targeted approaches to addressing their discomfort. Through a combination of awareness training, specific exercises, professional guidance, and lifestyle modifications, most people can achieve significant improvements in both comfort and function.
The journey toward optimal pelvic alignment and spinal health typically requires patience and consistency, but the rewards—reduced pain, improved movement capacity, and enhanced quality of life—make the effort worthwhile. By addressing these foundational aspects of human movement, individuals can build a stronger platform for all physical activities while reducing their risk of recurrent problems in the future.
Remember that each person’s path to improvement will be unique, reflecting their specific imbalances, history, and goals. This individualized approach, rather than generic solutions, offers the greatest potential for lasting relief from lower back pain associated with pelvic misalignment.
Click Hear for more tools :
1. What causes lower back pain and pelvic discomfort?
Lower back and pelvic pain can result from poor posture, muscle strain, herniated discs, pregnancy, arthritis, or conditions like sciatica or endometriosis.
2. How can I tell if my pelvic pain is related to my lower back?
If you experience pain that radiates from your lower back to your hips, groin, or legs, it may be connected. A healthcare professional can help diagnose the source.
3. What are the best home remedies for relieving this pain?
Gentle stretching, applying heat or cold, over-the-counter pain relievers, and rest can help ease mild lower back and pelvic pain.
4. When should I see a doctor for lower back and pelvic pain?
See a doctor if the pain lasts more than a few days, worsens, interferes with daily activities, or is accompanied by numbness, fever, or bladder issues.
5. Can physical therapy help with lower back and pelvic problems?
Yes, physical therapy is often very effective. Therapists can teach you exercises and posture adjustments that relieve pain and strengthen your core muscles.